A cancer treatment that is currently available to only a limited number of UK patients is to be tested in a clinical trial to see if it causes fewer long-term side effects than standard radiotherapy.
The brain cancer trial, which is now recruiting patients in Leeds, Manchester, Oxford, London, Cambridge and Kent*, will determine whether proton beam therapy can reduce the long-term side effects of radiotherapy and improve quality of life of patients compared with photon radiotherapy, the current standard treatment used globally.
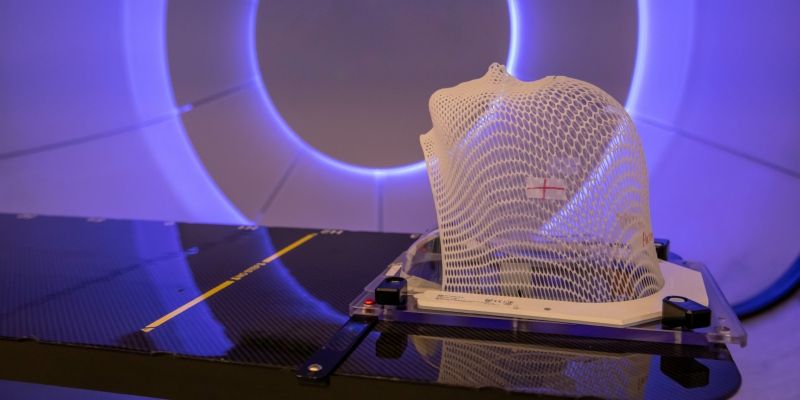
The technology uses a beam of a highly charged proton particles to destroy cancer cells. It does this by releasing a powerful burst of energy at the tumour site and delivers less radiation to the surrounding normal tissues.
The clinical trial, called APPROACH, funded by the National Institute for Health and Care Research (NIHR) and led by the University of Leeds, is open to patients with a type of brain cancer called oligodendroglioma that is diagnosed in about 350 UK patients per year. APPROACH stands for Analysis of Proton vs Photon Radiotherapy in Oligodendroglioma and Assessment of Cognitive Health.
The trial is academically co-led by Dr Louise Murray, Yorkshire Cancer Research Associate Professor and Honorary Consultant Clinical Oncologist, and Professor Susan Short, Professor of Neuro-Oncology, both from the University of Leeds’s School of Medicine.
This trial is vital to determine how we can use radiotherapy treatments appropriately, to give patients the best possible future.
It will be delivered through the University of Leeds Cancer Research UK Clinical Trials Unit, led by Professor Sarah Brown. Specialist teams at University College London Hospitals NHS Foundation Trust (UCLH) and The Christie NHS Foundation Trust in Manchester – the two UK proton beam therapy treatment centres – will lead on the development and delivery of proton beam therapy for this new clinical indication and support patients and families through treatment.
Dr Murray said: “We really need to know if this new technique can help reduce damage to the healthy brain tissue that surrounds a tumour, so that fewer patients have their lives affected by cognitive problems, such as difficulties with memory and processing information; problems like these can have a huge impact on daily life.
“This trial is vital to determine how we can use radiotherapy treatments appropriately, to give patients the best possible future.”
Protons vs photons
In the UK, standard radiotherapy is considered to be the most appropriate and effective treatment for the majority of cancers that are responsive to radiation treatment. It uses x-ray photons to destroy cancer cells, a technique which has been used successfully for more than 100 years, with continuous improvement resulting in greater accuracy and precision. Proton beam therapy is a relatively new technology in the UK. The NHS has invested in two major high energy proton beam radiotherapy centres and patients who receive proton beam therapy in the APPROACH trial will receive it at The Christie NHS Foundation Trust in Manchester, or University College London Hospitals NHS Foundation Trust (UCLH).
Proton beam therapy is only available to a small number of patients in the UK and up until 2018 could only be accessed abroad. Now it is available in the NHS at The Christie NHS Foundation Trust in Manchester and UCLH.
Current clinical indications for proton beam therapy have focused on where there are benefits over standard treatment, particularly where tumours are close to vital or delicate parts of the body, and some children’s cancers. More clinical research is required to understand how proton beam therapy compares with other treatment modalities to ensure the best treatment is selected for patients and is why this trial will play an important role in addressing some of these questions.
In both proton beam therapy and photon radiotherapy some damage may be caused to healthy tissue by the radiation beam inside the patient. In the case of photon radiotherapy, this also includes healthy tissue behind the tumour, since the x-rays continue to pass through the body beyond the tumour, albeit with less energy. Proton beam therapy may reduce the side effects from radiotherapy treatment because the beam of protons delivers a large burst of energy at the tumour site, with significantly less radiotherapy deposited beyond the tumour.
Dr Murray said: “We need high quality clinical trials to determine whether proton beam therapy is a better treatment for certain cancers. Clinical trials such as APPROACH are therefore of critical importance. Although we have some data to suggest that proton beam therapy might reduce long-term side effects, it is essential that we directly compare the two treatment approaches, and this will determine how future patients are best treated.”
Dr Naomi Fersht, consultant clinical oncologist at UCLH and one of the APPROACH trial investigators, said: “We are keen to begin this important trial and hope to be able to show that the use of proton beam therapy can minimise some of the side effects of radiotherapy for adult brain cancer patients. APPROACH is an example of the type of research we are now able to invite UK patients to participate in, working in collaboration with our partners nationally.”
Recruiting in 2024
Professor Nick Lemoine CBE, from the National Institute for Health & Care Research, which is funding the trial, said: “The launch of proton beam therapy in the UK is a major milestone in cancer care, but we need evidence for how best it can be used and that can only come from high quality clinical trials such as APPROACH.”
The trial will ultimately be open to patients from up to 18 recruiting cancer centres across the UK. Those taking part will be randomly assigned to receive either standard photon radiotherapy or proton beam therapy, so the side effects can be compared. Patients interested in joining the trial should contact their treating clinician to discuss suitability.
The APPROACH trial team has worked closely with brain tumour patients and their relatives, as well as staff working at The Christie, UCLH and the Leeds Cancer Research UK Clinical Trials Unit, in designing the trial. The National Cancer Research Institute Clinical Trials Radiotherapy Research Working Group (CTRad) provided expert support and guidance throughout the trial design process to ensure the trial would be efficient and of high quality. CTRad, now closed, brought the UK radiotherapy research community together to create world-leading large scale randomised trials that directly compare standard photon and proton beam radiotherapy.
David Sebag-Montefiore, Professor of Clinical Oncology and Health Research at Leeds’ School of Medicine and former CTRad Chair, said: “The APPROACH trial will answer critically important questions for brain cancer patients regarding the use of proton beam therapy. We hope that this treatment will improve quality of life for patients and reduce the long-term side effects they can often face.”
Dr Helen Bulbeck is co-founder of UK brain tumour charity brainstrust, and former patient representative for proton beam therapy in CTRad. She said: “This trial is so important and will help to dispel the myths that have developed about proton beam therapy.
“People need to be able to make informed decisions about their treatment choices. To do this we need the evidence that this trial will produce. This will put people in the driving seat, enabling them to be co-pilots in their care and the decisions they make.”
The trial will follow up with patients to assess their side effects, quality of life and survival rates for five years after treatment. The researchers hope that the trial results will lead to improved care and outcomes for patients with brain cancer and will help inform treatment of other cancers in the years to come.
Further information
For media requests please email University of Leeds press officer Lauren Ballinger via l.ballinger@leeds.ac.uk.
The trial is being funded by an investment of £1.5 million from the Efficacy and Mechanism Evaluation (EME) Programme - an NIHR and MRC partnership. National Institute for Health and Care Research and will open for recruitment of patients in 2023.
More information about the Leeds CRUK Clinical Trials Unit is available on the University of Leeds website.